Head and Neck Cancers
What are cancers of the head and neck?
Cancers that are known collectively as head and neck cancers usually begin in the squamous cells that line the mucosal surfaces of the head and neck (for example, those inside the mouth, throat, and voice box). These cancers are referred to as squamous cell carcinomas of the head and neck. Head and neck cancers can also begin in the salivary glands, sinuses, or muscles or nerves in the head and neck, but these types of cancer are much less common than squamous cell carcinomas (1, 2).
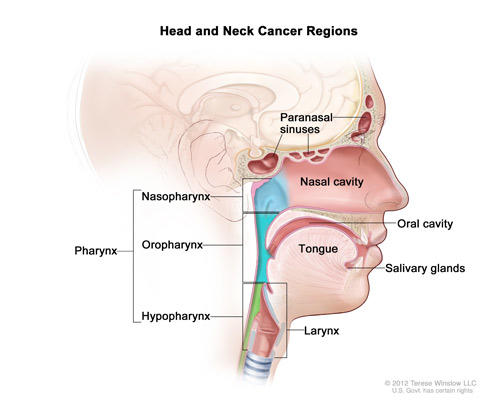
Cancers of the head and neck can form in the:
Oral cavity: Includes the lips, the front two-thirds of the tongue, the gums, the lining inside the cheeks and lips, the floor (bottom) of the mouth under the tongue, the hard palate (bony top of the mouth), and the small area of the gum behind the wisdom teeth.
Throat (pharynx): The pharynx is a hollow tube about 5 inches long that starts behind the nose and leads to the esophagus. It has three parts: the nasopharynx (the upper part of the pharynx, behind the nose); the oropharynx (the middle part of the pharynx, including the soft palate [the back of the mouth], the base of the tongue, and the tonsils); the hypopharynx (the lower part of the pharynx).
Voice box (larynx): The voice box is a short passageway formed by cartilage just below the pharynx in the neck. The voice box contains the vocal cords. It also has a small piece of tissue, called the epiglottis, which moves to cover the voice box to prevent food from entering the air passages.
Paranasal sinuses and nasal cavity: The paranasal sinuses are small hollow spaces in the bones of the head surrounding the nose. The nasal cavity is the hollow space inside the nose.
Salivary glands: The major salivary glands are in the floor of the mouth and near the jawbone. The salivary glands produce saliva. Minor salivary glands are located throughout the mucous membranes of the mouth and throat.
Head and neck cancer regions. Illustrates location of paranasal sinuses, nasal cavity, oral cavity, tongue, salivary glands, larynx, and pharynx (including the nasopharynx, oropharynx, and hypopharynx).
Credit: Terese Winslow
Cancers of the brain, the eye, the esophagus, the thyroid gland, and the skin of the head and neck are not usually classified as head and neck cancers.
If a squamous cell carcinoma of the head and neck is going to spread, it almost always does so locally and/or to the lymph nodes in the neck. Sometimes, cancerous squamous cells can be found in the lymph nodes of the upper neck when there is no evidence of cancer in other parts of the head and neck, possibly because the original primary tumor is too small. When this happens, the cancer is called metastatic squamous cell carcinoma with unknown (occult) primary. More information about this cancer type can be found in the Metastatic Squamous Neck Cancer with Occult Primary (PDQ®) cancer treatment summary.
What causes cancers of the head and neck?
Alcohol and tobacco use (including secondhand smoke and smokeless tobacco, sometimes called “chewing tobacco” or “snuff”) are the two most important risk factors for head and neck cancers, especially cancers of the oral cavity, hypopharynx, and voice box (3–7). People who use both tobacco and alcohol are at greater risk of developing these cancers than people who use either tobacco or alcohol alone (8, 9). Most head and neck squamous cell carcinomas of the mouth and voice box are caused by tobacco and alcohol use (8).
Infection with cancer-causing types of human papillomavirus (HPV), especially HPV type 16, is a risk factor for oropharyngeal cancers that involve the tonsils or the base of the tongue (10–12). In the United States, the incidence of oropharyngeal cancers caused by HPV infection is increasing, while the incidence of oropharyngeal cancers related to other causes is falling (10). About three-quarters of all oropharyngeal cancers are caused by chronic HPV infection (13, 14). Although HPV can be detected in other head and neck cancers, it appears to be the cause of cancer formation only in the oropharynx. The reasons for this are poorly understood.
Other known risk factors for specific cancers of the head and neck include the following:
Paan (betel quid). The use of paan (betel quid) in the mouth, a common custom in Southeast Asia, is strongly associated with an increased risk of mouth cancers (15, 16).
Occupational exposure. Occupational exposure to wood dust is a risk factor for nasopharyngeal cancer (17, 18). Certain industrial exposures, including exposures to asbestos and synthetic fibers, have been associated with cancer of the voice box, but the increase in risk remains controversial (19). People working in certain jobs in the construction, metal, textile, ceramic, logging, and food industries may have an increased risk of cancer of the voice box (20). Industrial exposure to wood dust, nickel dust, or formaldehyde is a risk factor for cancers of the paranasal sinuses and nasal cavity (21–23).
Radiation exposure. Radiation to the head and neck, for noncancerous conditions or cancer, is a risk factor for cancer of the salivary glands (24–26).
Epstein-Barr virus infection. Infection with the Epstein-Barr virus is a risk factor for nasopharyngeal cancer (27) and cancer of the salivary glands (28, 29).
Ancestry. Asian ancestry, particularly Chinese ancestry, is a risk factor for nasopharyngeal cancer (17, 18).
Underlying genetic disorders. Some genetic disorders, such as Fanconi anemia, can increase the risk of developing precancerous lesions and cancers early in life (30).
What are head and neck cancer symptoms?
Head and neck cancer symptoms may include a lump in the neck or a sore in the mouth or the throat that does not heal and may be painful, a sore throat that does not go away, difficulty in swallowing, and a change or hoarseness in the voice. These symptoms may also be caused by other, less serious conditions. It is important to check with a doctor or dentist about any of these symptoms.
Symptoms of cancers in specific areas of the head and neck include:
Oral cavity. A white or red patch on the gums, the tongue, or the lining of the mouth; a growth or swelling of the jaw that causes dentures to fit poorly or become uncomfortable; and unusual bleeding or pain in the mouth.
Throat (pharynx). Pain when swallowing; pain in the neck or the throat that does not go away; pain or ringing in the ears; or trouble hearing.
Voice box (larynx). Trouble breathing or speaking, pain when swallowing or ear pain.
Paranasal sinuses and nasal cavity. Sinuses that are blocked and do not clear; chronic sinus infections that do not respond to treatment with antibiotics; bleeding through the nose; frequent headaches, swelling or other trouble with the eyes; pain in the upper teeth; or problems with dentures.
Salivary glands. Swelling under the chin or around the jawbone, numbness or paralysis of the muscles in the face, or pain in the face, the chin, or the neck that does not go away.
How common are head and neck cancers?
Head and neck cancers account for nearly 4% of all cancers in the United States (31).
These cancers are more than twice as common among men as they are among women (31). Head and neck cancers are also diagnosed more often among people over age 50 than they are among younger people.
Researchers estimated that more than 68,000 men and women in the United States would be diagnosed with head and neck cancers in 2021 (31). Most will be diagnosed with mouth, throat, or voice box cancer. Paranasal sinus and nasal cavity cancer and salivary gland cancer are much less common.
How can I reduce my risk of developing head and neck cancers?
People who are at risk of head and neck cancers―particularly those who use tobacco―should talk with their doctor about ways to stop using tobacco to reduce their risk.
Avoiding oral HPV infection can reduce the risk of HPV-associated head and neck cancers. In June 2020, the Food and Drug Administration granted accelerated approval of the HPV vaccine Gardasil 9 for the prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58 in persons aged 9 through 45 years. More information about these vaccines is available in the Human Papillomavirus (HPV) Vaccines fact sheet.
Although there is no standard or routine screening test for head and neck cancers, dentists may check the oral cavity for signs of cancer during a routine checkup.
How are head and neck cancers treated?
Head and neck cancer treatment can include surgery, radiation therapy, chemotherapy, targeted therapy, immunotherapy, or a combination of treatments. The treatment plan for an individual patient depends on a number of factors, including the location of the tumor, the stage of the cancer, and the person’s age and general health.
Research has shown that patients with HPV-positive oropharyngeal tumors have a much better prognosis and higher chance of complete cure than those with HPV-negative tumors following the same treatment (32). Because of this, ongoing clinical trials are investigating whether patients with HPV-positive cancers can be treated with less intensive regimens, such as less intensive radiation or immunotherapy.
More information about head and neck cancer treatment is in the PDQ® cancer treatment summaries for specific types of head and neck cancer:
- Hypopharyngeal Cancer
- Laryngeal Cancer
- Lip and Oral Cavity Cancer
- Metastatic Squamous Neck Cancer with Occult Primary
- Nasopharyngeal Cancer
- Oropharyngeal Cancer
- Paranasal Sinus and Nasal Cavity Cancer
- Salivary Gland Cancer
Patients and their doctors should consider treatment options carefully. They should discuss each type of treatment and how it might change the way the patient looks, talks, eats, or breathes and how each treatment can affect their quality of life.
What are the side effects of head and neck cancer treatment?
Surgery for head and neck cancers may affect the patient’s ability to chew, swallow, or talk. The patient may look different after surgery, and the face and neck may be swollen. The swelling usually improves with time. However, if lymph nodes are removed, the flow of lymph in the area where they were removed may be slower and lymph could collect in the tissues (a condition called lymphedema), causing additional swelling that may last for a long time.
Head and neck lymphedema may be visible or internal. In most cases, it can be reversed, improved, or reduced if treated promptly. Patients with untreated lymphedema may be more at risk of complications such as cellulitis, or an infection of the tissues. Untreated cellulitis, if severe, can be dangerous and could lead to further swallowing or breathing difficulties.
After a laryngectomy (surgery to remove the voice box) or other surgery in the neck, parts of the neck and throat may feel numb because nerves have been cut. If lymph nodes in the neck were removed, the shoulder and neck may become weak and stiff.
Patients who receive radiation to the head and neck may experience side effects during and for a short while after treatment, including redness, irritation, and sores in the mouth; a dry mouth or thickened saliva; difficulty in swallowing; changes in taste; or nausea. Radiation may also cause loss of taste, which may decrease appetite and affect nutrition, and earaches (caused by the hardening of ear wax). Patients may also notice some swelling or drooping of the skin under the chin and changes in the texture of the skin. The jaw may feel stiff, and patients may not be able to open their mouth as wide as before treatment.
Although side effects will improve slowly over time in many patients, others will experience long-term side effects of surgery or radiation therapy, including difficulty swallowing, speech impairment, and skin changes (33).
Patients should report any side effects to their doctor or nurse and discuss how to deal with them.
What rehabilitation or support options are available for patients with head and neck cancers?
The goal of treatment for head and neck cancers is to control the disease. But doctors are also concerned about preserving the function of the affected areas as much as they can and helping the patient return to normal activities as soon as possible after treatment. Rehabilitation is a very important part of this process. The goals of rehabilitation depend on the extent of the disease and the treatment that a patient has received.
Depending on the location of the cancer and the type of treatment, rehabilitation may include physical therapy, dietary counseling, speech therapy, and/or learning how to care for a stoma. A stoma is an opening into the windpipe through which a patient breathes after a laryngectomy, which is surgery to remove the voice box. The National Library of Medicine has more information about laryngectomy in MedlinePlus.
Sometimes, especially with cancer of the oral cavity, a patient may need reconstructive and plastic surgery to rebuild bones or tissues. However, reconstructive surgery may not always be possible because of damage to the remaining tissue from the original surgery or from radiation therapy. If reconstructive surgery is not possible, a prosthodontist may be able to make a prosthesis (an artificial dental and/or facial part) to restore satisfactory swallowing, speech, and appearance. Patients will receive special training on how to use the device.
Patients who have trouble speaking after treatment may need speech therapy. Often, a speech-language pathologist will visit the patient in the hospital to plan therapy and teach speech exercises or alternative methods of speaking. Speech therapy usually continues after the patient returns home.
Eating may be difficult after treatment for head and neck cancer. Some patients receive nutrients directly into a vein after surgery or need a feeding tube until they can eat on their own. A feeding tube is a flexible plastic tube that is passed into the stomach through the nose or an incision in the abdomen. A nurse or speech-language pathologist can help patients learn how to swallow again after surgery.
Is follow-up care necessary? What does it involve?
Regular follow-up care is very important after treatment for head and neck cancer to make sure that the cancer has not returned and that a second primary (new) cancer has not developed. Head and neck cancers not related to HPV infection are especially likely to recur after treatment. Depending on the type of cancer, medical check-ups could include exams of the stoma, if one has been created, and of the mouth, neck, and throat. Regular dental exams may also be necessary.
From time to time, the doctor may perform a complete physical exam, blood tests, x-rays, and computed tomography (CT), positron emission tomography (PET), or magnetic resonance imaging (MRI) scans. The doctor may monitor thyroid and pituitary gland function, especially if the head or neck was treated with radiation. Also, the doctor is likely to counsel patients to stop smoking. Research has shown that continued smoking by a patient with head and neck cancer may reduce the effectiveness of treatment and increase the chance of a second primary cancer.
Additional information can be found at NCI’s Follow-Up Medical Care page.
How can people who have had head and neck cancers reduce their risk of developing a second primary (new) cancer?
People who have been treated for head and neck cancers have an increased chance of developing a new cancer, usually in the head, neck, esophagus, or lungs (34–36). The chance of a second primary (new) cancer varies depending on the site of the original cancer, but it is higher for people who use tobacco and drink alcohol (34).
Especially because patients who smoke have a higher risk of a second primary cancer, doctors encourage patients who use tobacco to quit. Information about tobacco cessation is available from NCI’s Cancer Information Service at 1-800-4-CANCER (1-800-422-6237) and at smokefree.gov. The toll-free number 1-800-QUIT-NOW (1-800-784-8669) also serves as a single point of access to state-based telephone quit lines.
Call NCI’s Cancer Information Service at 1-800-4-CANCER (1-800-422-6237) for information about clinical trials for treatment of head and neck cancer.
Selected References
- Chow LQM. Head and neck cancer. New England Journal of Medicine 2020; 382(1):60–72. doi:10.1056/NEJMra1715715
Son E, Panwar A, Mosher CH, Lydiatt D. Cancers of the major salivary gland. Journal of Oncology Practice 2018; 14(2):99–108.
Gandini S, Botteri E, Iodice S, et al. Tobacco smoking and cancer: a meta-analysis. International Journal of Cancer 2008; 122(1):155–164.
Hashibe M, Boffetta P, Zaridze D, et al. Evidence for an important role of alcohol- and aldehyde-metabolizing genes in cancers of the upper aerodigestive tract. Cancer Epidemiology, Biomarkers and Prevention 2006; 15(4):696–703.
Hashibe M, Brennan P, Benhamou S, et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Journal of the National Cancer Institute 2007; 99(10):777–789.
Boffetta P, Hecht S, Gray N, Gupta P, Straif K. Smokeless tobacco and cancer. The Lancet Oncology 2008; 9(7):667–675.
Mariano LC, Warnakulasuryia S, Straif K, Monteiro L. Secondhand smoke exposure and oral cancer risk: A systematic review and meta-analysis. Tobacco Control 2021:tobaccocontrol-2020-056393. doi: 10.1136/tobaccocontrol-2020-056393.
Hashim D, Genden E, Posner M, Hashibe M, Boffetta P. Head and neck cancer prevention: From primary prevention to impact of clinicians on reducing burden. Annals of Oncology 2019; 30(5):744–756.
Hashibe M, Brennan P, Chuang SC, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: Pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiology, Biomarkers and Prevention 2009; 18(2):541–550.
Chaturvedi AK, Engels EA, Pfeiffer RM, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. Journal of Clinical Oncology 2011; 29(32)4294–4301.
Adelstein DJ, Ridge JA, Gillison ML, et al. Head and neck squamous cell cancer and the human papillomavirus: Summary of a National Cancer Institute State of the Science Meeting, November 9–10, 2008, Washington, D.C. Head and Neck 2009; 31(11):1393–1422.
Gillison ML, D’Souza G, Westra W, et al. Distinct risk factors profiles for human papillomavirus type 16-positive and human papillomavirus type-16 negative head and neck cancers. Journal of the National Cancer Institute 2008; 100(6):407–420.
Saraiya M, Unger ER, Thompson TD, et al. US assessment of HPV types in cancers: Implications for current and 9-valent HPV vaccines. Journal of the National cancer Institute 2015; 107(6):djv086. doi: 10.1093/jnci/djv086.
Senkomago V, Henley SJ, Thomas CC, et al. Human papillomavirus-attributable cancers - United States, 2012–2016. MMWR. Morbidity and Mortality Weekly Report 2019; 68(33):724–728.
Ho PS, Ko YC, Yang YH, Shieh TY, Tsai CC. The incidence of oropharyngeal cancer in Taiwan: An endemic betel quid chewing area. Journal of Oral Pathology and Medicine 2002; 31(4):213–219.
Goldenberg D, Lee J, Koch WM, et al. Habitual risk factors for head and neck cancer. Otolaryngology and Head and Neck Surgery 2004; 131(6):986–993.
- Yu MC, Yuan JM. Nasopharyngeal Cancer. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
Yu MC, Yuan JM. Epidemiology of nasopharyngeal carcinoma. Seminars in Cancer Biology 2002; 12(6):421–429.
- Olshan AF. Cancer of the Larynx. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
Boffetta P, Richiardi L, Berrino F, et al. Occupation and larynx and hypopharynx cancer: An international case–control study in France, Italy, Spain, and Switzerland. Cancer Causes and Control 2003; 14(3):203–212.
- Littman AJ, Vaughan TL. Cancers of the Nasal Cavity and Paranasal Sinuses. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
Luce D, Leclerc A, Bégin D, et al. Sinonasal cancer and occupational exposures: A pooled analysis of 12 case–control studies. Cancer Causes and Control 2002; 13(2):147–157.
Luce D, Gérin M, Leclerc A, et al. Sinonasal cancer and occupational exposure to formaldehyde and other substances. International Journal of Cancer 1993; 53(2):224–231.
- Mayne ST, Morse DE, Winn DM. Cancers of the Oral Cavity and Pharynx. In: Schottenfeld D, Fraumeni JF Jr., editors. Cancer Epidemiology and Prevention. 3rd ed. New York: Oxford University Press, 2006.
Preston-Martin S, Thomas DC, White SC, Cohen D. Prior exposure to medical and dental x-rays related to tumors of the parotid gland. Journal of the National Cancer Institute 1988; 80(12):943–949.
Horn-Ross PL, Ljung BM, Morrow M. Environmental factors and the risk of salivary gland cancer. Epidemiology 1997; 8(4):414–429.
Chien YC, Chen JY, Liu MY, et al. Serologic markers of Epstein-Barr virus infection and nasopharyngeal carcinoma in Taiwanese men. New England Journal of Medicine 2001; 345(26):1877–1882.
Hamilton-Dutoit SJ, Therkildsen MH, Neilsen NH, et al. Undifferentiated carcinoma of the salivary gland in Greenlandic Eskimos: Demonstration of Epstein-Barr virus DNA by in situ nucleic acid hybridization. Human Pathology 1991; 22(8):811–815.
Chan JK, Yip TT, Tsang WY, et al. Specific association of Epstein-Barr virus with lymphoepithelial carcinoma among tumors and tumorlike lesions of the salivary gland. Archives of Pathology and Laboratory Medicine 1994; 118(10):994–997.
Beddok A, Krieger S, Castera L, Stoppa-Lyonnet D, Thariat J. Management of Fanconi anemia patients with head and neck carcinoma: Diagnosis and treatment adaptation. Oral Oncology 2020; 108:104816.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA: A Cancer Journal for Clinicians 2021; 71(1):7–33.
Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. New England Journal of Medicine 2010; 363(1):24–35.
Strojan P, Hutcheson KA, Eisbruch A, et al. Treatment of late sequelae after radiotherapy for head and neck cancer. Cancer Treatment Reviews 2017;59:79–92.
Do KA, Johnson MM, Doherty DA, et al. Second primary tumors in patients with upper aerodigestive tract cancers: Joint effects of smoking and alcohol (United States). Cancer Causes and Control 2003; 14(2):131–138.
Argiris A, Brockstein BE, Haraf DJ, et al. Competing causes of death and second primary tumors in patients with locoregionally advanced head and neck cancer treated with chemoradiotherapy. Clinical Cancer Research 2004; 10(6)1956–1962.
Chuang SC, Scelo G, Tonita JM, et al. Risk of second primary cancer among patients with head and neck cancers: A pooled analysis of 13 cancer registries. International Journal of Cancer 2008; 123(10):2390–2396.
Posted:
Updated:
Reviewed:
This content is provided by the National Cancer Institute (www.cancer.gov)
Source URL: https://www.cancer.gov/node/12879/syndication
Source Agency: National Cancer Institute (NCI)
Captured Date: 2013-12-06 15:00:03.0